

October: A Month for Women’s Comprehensive Health in Mexico
Breast cancer is the most common type of cancer among women, both in Mexico and globally. According to the Mexican Ministry of Health, thousands of new cases are diagnosed every year. Early detection is key—it significantly increases the chances of successful treatment and a better quality of life.
When and How to Perform Breast Exams
Self-Breast Exam
- When to start? From age 20.
- How often? Monthly, ideally 5 to 7 days after the start of your menstrual period when breasts are less sensitive.
- How to do it?
- In front of a mirror: Look for any changes in shape, size, symmetry, or skin texture, and observe for nipple changes.
- In the shower: Use the pads of your fingers to feel for lumps in circular motions, moving from the outer area toward the nipple, including the armpit.
- Lying down: Place a pillow under your shoulder and repeat the palpation process.
- Why it’s important: Becoming familiar with the normal look and feel of your breasts helps you detect any unusual changes early, which can then be assessed by a healthcare professional.
Clinical Breast Exam
- When to start? At age 25.
- Frequency: Every 1 to 3 years until age 40, then annually.
- What it involves: A healthcare provider performs a detailed physical exam to detect abnormalities that might not be noticed during self-exams.
Mammogram
- Recommended age:
- Average risk: Start between 40 and 45.
- High risk: Your doctor may suggest starting earlier.
- Frequency: Yearly or every two years, depending on medical advice and clinical guidelines.
- Why it matters: Mammograms are the most effective way to detect breast cancer in its early stages, even before symptoms appear.
Breast Ultrasound
- When is it recommended? In specific situations.
- When it’s used:
- Dense breasts: Ultrasound can complement mammograms to provide better imaging.
- Women under 30: It’s the first option for evaluating lumps, as mammograms are less effective for this group.
- Further evaluation: If an abnormality is detected in a mammogram, an ultrasound can help determine if it’s solid or fluid-filled.
MRI (Magnetic Resonance Imaging)
- For whom? Women at high risk of breast cancer, such as those with BRCA1 or BRCA2 mutations or a strong family history.
- Usage: Recommended in combination with annual mammograms starting at age 30.
The Importance of Family History
Knowing your family history is crucial for evaluating your personal risk:
- Key questions to ask:
- Does anyone in the family have breast or ovarian cancer?
- Who was affected? (Consider first-degree relatives like mothers, sisters, or daughters, and second-degree relatives like grandmothers and aunts.)
- At what age were they diagnosed? (A diagnosis before age 50 could indicate higher genetic risk.)
- Is the family history on your mother’s or father’s side? (Both sides are equally important.)
- Are there any known genetic mutations in the family, such as BRCA1 or BRCA2?
- Next steps if you have a family history:
- Genetic counseling: A geneticist can help determine whether you need genetic testing.
- Customized screening plan: You may need earlier and more frequent screening.
Additional Risk Factors
Besides family history, other factors can increase the risk of breast cancer:
- Age: Risk increases with age, especially after 50.
- Personal history: Previous breast cancer or other breast conditions.
- Lifestyle: Alcohol consumption, obesity, lack of physical activity, and poor diet.
- Hormonal factors: Early menstruation (before age 12), late menopause (after age 55), or prolonged hormone therapy.
Promoting Comprehensive Health
Prevention goes beyond early detection. A healthy lifestyle plays a vital role in maintaining well-being:
- Balanced diet: Focus on fruits, vegetables, whole grains, and minimize saturated fats.
- Physical activity: At least 150 minutes of moderate exercise per week.
- Avoid alcohol and smoking.
Women’s Health Checkups
We offer two health checkup options designed to cover key aspects of women’s health:
Basic Checkup
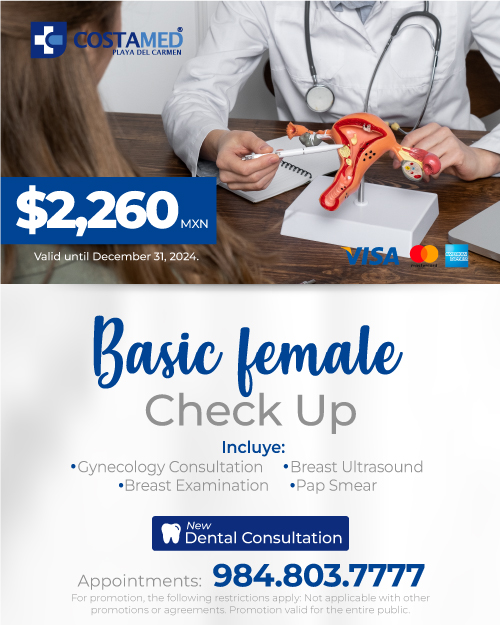
- Includes:
- Gynecological consultation: Comprehensive evaluation of sexual and reproductive health.
- Basic lab tests: Complete blood count, lipid profile, and glucose levels to detect conditions like anemia, high cholesterol, or diabetes.
- Pap smear: Early detection of cervical cancer and other abnormalities caused by HPV.
- Breast ultrasound: Additional imaging to detect cysts or masses.
- Benefits:
- Early detection: Identify health issues before symptoms appear.
- Personalized advice: Discuss concerns and receive tailored recommendations.
Extended Checkup
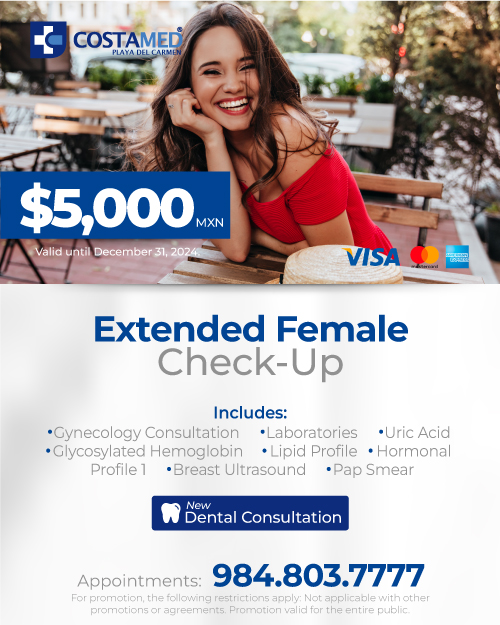
- Includes everything from the basic checkup, plus:
- Additional benefits:
- Hormonal profile: Evaluate thyroid function, estrogen, progesterone, and other hormone levels.
- Hormonal balance detection: Helps address menstrual irregularities, fertility issues, mood swings, and metabolic concerns.
- Reproductive health planning: Valuable information for contraception, pregnancy, and menopause management.
Steps Toward Optimal Health
- Schedule your appointment: Don’t wait for symptoms—prevention is key.
- Track your family history: Share it with your doctor for a more accurate risk assessment.
- Follow recommended screenings: Stay on schedule with health screenings.
- Adopt a healthy lifestyle: Focus on nutrition, exercise, and avoiding harmful habits.
- Stay informed and proactive: Education is your best tool for making informed decisions.
Available Resources
In Mexico, several programs and organizations are dedicated to women’s health:
- National Cancer Institute (INCan): Offers screening and treatment programs.
- Public Health Centers: Provide free or low-cost mammograms and Pap smears.
- Non-Governmental Organizations: Like Fundación CIMA, which supports women diagnosed with breast cancer.
October serves as an annual reminder of the importance of early breast cancer detection, but your health deserves continuous attention. By understanding when and how to perform exams, knowing your family history, and taking advantage of health checkups, you’re taking meaningful steps toward a healthier life.
Remember, prevention and self-care aren’t one-time actions—they’re ongoing commitments to yourself. Don’t hesitate to seek professional support or guidance for any concerns you may have.
Like it? Share it!